- Cushing’s disease occurs when there is too much of the steroid hormone cortisol in the blood level due to excessive ACTH hormone secretion by a pituitary tumor
- ACTH (adrenocorticotropic hormone) is a hormone produced by the normal pituitary gland. ACTH stimulates the adrenal glands (located on top of the kidneys) to produce cortisol
- Cushing’s disease occurs more commonly in adults. Most patients with Cushing’s disease have small tumors (pituitary microadenomas).
- The disease affects 10 to 15 people per million each year, most commonly adults ages 20 to 50. Women account for more than 70 percent of cases.
- The diagnosis of Cushing’s disease is often long delayed and can be difficult to make. An endocrinologist should always supervise the evaluation for Cushing’s disease.
- Cushing’s disease is not the same as Cushing’s syndrome. Cushing’s syndrome refers to the general state characterized by excessive levels of the steroid hormone cortisol in the blood. Elevated cortisol levels can occur for reasons other than a pituitary tumor, including:
- Tumors of the adrenal glands producing cortisol
- Certain types of cancer, elsewhere in the body, can make ACTH, which then stimulates the normal adrenal glands to make excessive cortisol. This is called “ectopic” ACTH production.
Symptoms
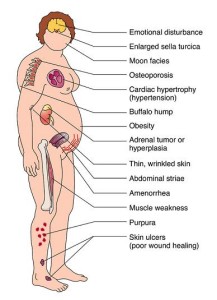
- Cushing’s disease (and Cushing’s syndrome) produce a wide range of symptoms, including:
- Changes in physical characteristics of the body
- Fullness and rounding of the face (so-called “moon facies”)
- Added fat on back of neck (so-called “buffalo hump”)
- Skin changes with easy bruising
- Purplish stretch marks on the abdomen (“abdominal striae”)
- Excessive weight gain
- Red cheeks
- Excess hair growth on the face, neck, chest, abdomen, and thighs
- Generalized weakness and fatigue; wasting of muscles
- Menstrual disorders
- Decreased fertility and/or sex drive
- High blood pressure
- Diabetes mellitus
- Mood and behavior disorders
Diagnosis
- Clinical Examination:
- The early stages of Cushing’s disease are difficult to recognize clinically, especially because the body changes come on slowly
- Comparison of old and recent photographs often shows the changes in facial appearance and physical characteristics of the body
- Pregnancy may worsen symptoms of Cushing’s disease which are commonly attributed to the pregancy state
- The early stages of Cushing’s disease are difficult to recognize clinically, especially because the body changes come on slowly
- Hormonal diagnosis:
- The first step in diagnosing Cushing’s disease is to confirm the presence of excessive cortisol secretion
- Blood levels of cortisol naturally vary throughout the day, and therefore blood cortisol level measurement alone is seldom definitive
- The amount of cortisol found in urine collected over a 24-hour period is typically an important measurement (the test is called a 24-hour urine free cortisol measurement)
- In some individuals with depression, alcohol abuse, anorexia nervosa or high estrogen levels, cortisol levels may be chronically elevated. These patients with “pseudo-Cushing’s” may be difficult to distinguish from those with true Cushing’s. Additional hormonal tests are often needed to clarify the diagnosis.
- By definition, ACTH blood levels are elevated in Cushing’s disease
- An elevated ACTH levels alone is not diagnostic for Cushing’s disease, since ACTH can be produced by cancerous tumors elsewhere in the body (ectopic ACTH production)
- Your endocrinologist may order a dexamethasone suppression test to help distinguish Cushing’s disease (pituitary) from ectopic ACTH production
- Dexamethasone is a powerful drug that acts similar to, but is more potent than cortisol.
- Normally, an excessively high blood cortisol level is detected by the brain, which in turn regulates the pituitary gland to decrease the production of ACTH.
- In normal individuals, 1 mg of dexamethasone will suppress ACTH production (lowering the ACTH level in the blood)
- The pituitary tumor cells producing ACTH in Cushing’s disease often also respond to the dexamethasone, leading to a temporary reduction in blood ACTH levels
- Ectopic ACTH production is not suppressed by dexamethasone
- Dexamethasone is a powerful drug that acts similar to, but is more potent than cortisol.
In some cases, MRI (see Imaging below) fails to identify an abnormality within the pituitary gland.
- The first step in diagnosing Cushing’s disease is to confirm the presence of excessive cortisol secretion
- If the diagnosis of Cushing’s disease is suspected, super-selective inferior petrosal sinus sampling (IPSS) may be ordered
- The inferior petrosal sinuses are veins that occur on both sides of the pituitary gland
- Blood leaving the right half of the pituitary gland drains into the right inferior petrosal sinus, and vice-versa
- Specially-trained interventional neuroradiologists are able to navigate a tiny catheter into the inferior petrosal sinus. Blood samples are then taken from each sinus, and also from a vein in the arm.
- If the ACTH level is much higher in one inferior petrosal sinus compared to the other, then this suggests that the tumor is on that side. Surgical exploration of the pituitary gland may be guided by this finding
- Another expected finding in Cushing’s disease is that the ACTH level in the inferior petrosal sinus should be higher than in the blood taken from the arm.
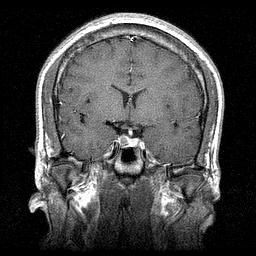
- Imaging:
- Once the diagnosis is suspected based on clinical findings and hormonal testing, a magnetic resonance imaging (MRI) scan of the pituitary glad is the best way to detect the presence of an adenoma in Cushing’s disease.
- MRI detects an adenoma in about 70 percent of cases. We have a powerful 1.5T MRI scanners that may offer improved chances of identifying very small tumors.
Treatment
- Surgery:
- Transsphenoidal surgeryto remove the adenoma offers the only long-term cure of Cushing’s disease.
- The cure rate for smaller tumors (microadenomas) is 80 percent to 85 percent.
- The cure rate is 50 percent to 55 percent for larger tumors that have spread into adjacent structures.
- Medical therapy:
- Medications that inhibit cortisol production in the adrenal gland —ketoconazole, aminoglutethimide, and metyrapone—can effectively treat cases where surgery fails, though all have some side effects.
- Radio-therapy:
- Both conventional (external beam) and stereotactic radiosurgery are treatment options if surgery fails. However, stereotactic radiosurgery typically is more effective with fewer side effects. External beam radiation causes loss of normal pituitary function over five to 10 years. Complications such as visual loss, weakness, and memory impairment occur on rare occasions with either option.