Simpy meaning craniotomy is opening the skull. Craniotomy is a very old procedure, even mentioned in medieval times! Offcourse, those times, skull was being cut with sharp stones and heavy metal objects while the patient is fully awake. Many patients never regained consciousness after surgery!
Gradual refinement in surgical techniques along with discovery of antibiotics have brought in much needed comfort for patients.
Craniotomy is performed for various diseases of the brain. Brain tumors, stroke, trigeminal neuralgia, brain injury are all managed with this technique. Lets consider it step by step.
Human craniotomy is usually performed under general anesthesia but can be also done with the patient awake using a local anaesthetic; the procedure typically does not involve significant discomfort for the patient. In general, a craniotomy will be preceded by an MRIscan which provides a picture of the brain that the surgeon uses to plan the precise location for bone removal and the appropriate angle of access to the relevant brain areas. The amount of skull that needs to be removed depends to a large extent on the type of surgery being performed.?
Skin incision
After the scalp is prepped with an antiseptic, a skin incision is made, usually behind the hairline.
The surgeon attempts to ensure a good cosmetic result after surgery. Sometimes a hair sparing technique can be used that requires shaving only a 1/4-inch wide area along the proposed incision. Sometimes the entire incision area may be shaved.
Opening the skull
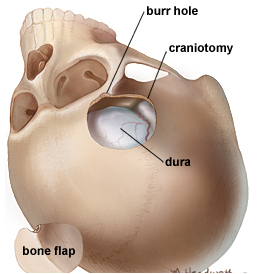
The skin and muscles are lifted off the bone and folded back. Next, one or more small burr holes are made in the skull with a drill. Inserting a special saw through the burr holes, the surgeon uses this craniotome to cut the outline of a bone flap.
The cut bone flap is lifted and removed to expose the protective covering of the brain called the dura. The bone flap is safely stored until it is replaced at the end of the procedure.
Exposure of the brain
After opening the dura with surgical scissors, the surgeon folds it back to expose the brain. Retractors placed on the brain gently open a corridor to the area needing repair or removal. Neurosurgeons use special magnification glasses, called loupes, or an operating microscope to see the delicate nerves and vessels.
Adressing the problem
Because the brain is tightly enclosed inside the bony skull, tissues cannot be easily moved aside to access and repair problems. Neurosurgeons use a variety of very small tools and instruments to work deep inside the brain.
These include long-handled scissors, dissectors and drills, lasers, ultrasonic aspirators (uses a vibrations to break up tumors and suck up the tumor), and computer image-guidance systems. In some cases, evoked potential monitoring is used to stimulate specific cranial nerves while the response is monitored in the brain. This is done to preserve function of the nerve and make sure it is not further damaged during surgery.
Closure of the craniotomy wound
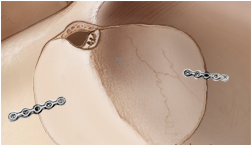
With the problem removed or repaired, the retractors holding the brain are removed and the dura is closed with sutures. The bone flap is replaced back in its original position and secured to the skull with titanium plates and screws
The plates and screws remain permanently to support the area; these can sometimes be felt under your skin. In some cases, a drain may be placed under the skin for a couple of days to remove blood or fluid from the surgical area. The muscles and skin are sutured back together. A soft adhesive dressing is placed over the incision.
What happens after surgery?
After surgery, you are taken to the recovery room where vital signs are monitored as you awake from anesthesia. The breathing tube (ventilator) usually remains in place until you fully recover from the anesthesia. Next, you are transferred to the neuro intensive care unit (NSICU) for close observation and monitoring. You are frequently asked to move your arms, fingers, toes, and legs.
A nurse will check your pupils with a flashlight and ask questions, such as “What is your name?” You may experience nausea and headache after surgery; medication can control these symptoms. Depending on the type of brain surgery, steroid medication (to control brain swelling) and anticonvulsant medication (to prevent seizures) may be given. When your condition stabilizes, you’ll be transferred to a regular room where you’ll continue to be monitored and begin to increase your activity level.
The length of the hospital stay varies, from only 2 to 7 days depending on the surgery and development of any complications. When released from the hospital, you’ll be given discharge instructions. Stitches or staples are removed 7–10 days after surgery in the doctor’s office.
Discomfort
Discomfort- After surgery, headache pain is managed with a narcotic medication. Thereafter, pain is managed with acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., aspirin; ibuprofen).
- A medicine (anticonvulsant) may be prescribed temporarily to prevent seizures. Common anticonvulsants include Dilantin (phenytoin), Tegretol (carbamazepine). Some patients develop side effects (e.g., drowsiness, balance problems, rashes) caused by these anticonvulsants. In these cases, blood samples are taken to monitor the drug levels and manage the side effects.
Restrictions
- Do not drive after surgery until discussed with your surgeon and avoid sitting for long periods of time.
- Do not lift anything heavier than 5 kg including children.
- Housework is not permitted until the first follow-up office visit. (gardening, mowing, vacuuming, ironing, and loading/unloading the dishwasher, washer, or dryer.)
- Do not drink alcoholic beverages.
Activity
- Gradually return to your normal activities. Fatigue is common.
- An early exercise program to gently stretch the neck and back may be advised.
- Walking is encouraged; start with short walks and gradually increase the distance. Wait to participate in other forms of exercise until discussed with your surgeon.
Bathing/Incision Care
- You may shower and shampoo 3 to 4 days after surgery unless otherwise directed by your surgeon.
- Sutures or staples, which remain in place when you go home, will need to be removed 7 to 14 days after surgery. Ask your surgeon or call the office to find out when.
When to Call Your Doctor
If you experience any of the following:
- A temperature that exceeds 101º F
- An incision that shows signs of infection, such as redness, swelling, pain, or drainage.
- If you are taking an anticonvulsant, and notice drowsiness, balance problems, or rashes.
- Decreased alertness, increased drowsiness, weakness of arms or legs, increased headaches, vomiting, or severe neck pain that prevents lowering your chin toward the chest.
Recovery
The recovery time varies from 1 to 4 weeks depending on the underlying disease being treated and your general health. Full recovery may take up to 8 weeks. Walking is a good way to begin increasing your activity level. Start with short, frequent walks within the house and gradually try walks outside. It’s important not to overdo it, especially if you are continuing treatment with radiation or chemotherapy. Ask your surgeon when you can expect to return to work.
What are the risks?
No surgery is without risks. General complications of any surgery include bleeding, infection, blood clots, and reactions to anesthesia. Specific complications related to a craniotomy may include:
- stroke
- seizures
- swelling of the brain, which may require a second craniotomy
- nerve damage, which may cause muscle paralysis or weakness
- CSF leak, which may require repair
- loss of mental functions
- permanent brain damage with associated disabilities
What are the results?
The results of your craniotomy depend on the underlying condition being treated.